Modern Aspects of Analgosedation in Critically ill Patients

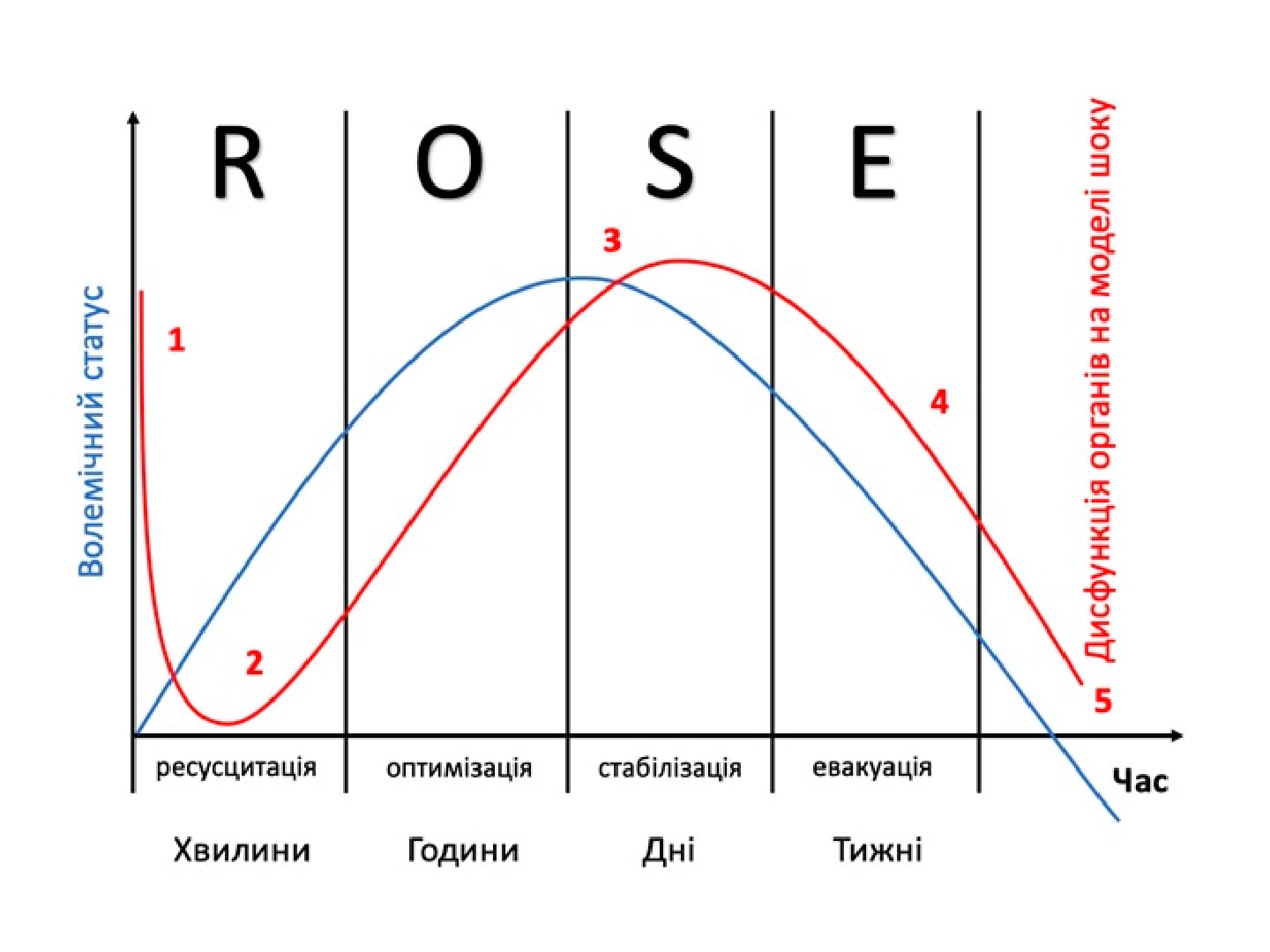
Abstract. Introduction. In contemporary intensive care units, clinical practice is shifting from prolonged deep sedation with benzodiazepines and opioids toward lighter, controlled, and «cooperative» sedation. This change is driven by the association of deep sedation with an increased risk of delirium, longer duration of mechanical ventilation, higher mortality, and adverse long-term outcomes. At the same time, the role of analgosedation with minimal use of benzodiazepines and an emphasis on maintaining patient interaction is increasing.
The aim of this work is to summarize modern aspects of analgosedation in critically ill patients, focusing on the pharmacological properties of midazolam and dexmedetomidine and analyzing their use in anesthesiology and intensive care.
The objectives of the work are to outline the evolution of sedation approaches in intensive care units, to describe the pharmacodynamic and pharmacokinetic characteristics of midazolam, to analyze its potential for sedation of varying depth, and to compare it with the effects of dexmedetomidine. The article also considers the specific features of using these agents in clinical situations requiring prolonged, controlled, or sequential sedation.
Keywords: analgosedation; critically ill patients; midazolam; dexmedetomidine; benzodiazepines; cooperative sedation; intensive care unit; mechanical ventilation; delirium.
Authors:
- Kobelyatskyi Y.Y. Dnipro State Medical University, Ukraine.
Conclusions:
Analgosedation is a key component of managing critically ill patients, and modern approaches aim to reduce the depth of sedation and avoid the routine use of benzodiazepines. Midazolam remains an important agent for short-term sedation, induction of anesthesia, anterograde amnesia, rescue sedation, and control of anxiety and seizures, although analgosedation generally requires its combination with opioids. Dexmedetomidine provides dose-dependent sedation while preserving patient interaction, has minimal respiratory depressive effects, modulates sleep and sympathetic activity, and can be used in sepsis, septic shock, delirium, and withdrawal states, which aligns with modern con-cepts of cooperative sedation. Sequential use of midazolam and dexmedetomidine may be effective when prolonged sedation is required in selected patients.
Literature:
- Petty TL. Suspended life or extending death? Chest. 1998;114(2):360–1. doi: 10.1378/chest.114.2.360
- Barr J, Fraser GL, Puntillo K, Ely EW, Gelinas C, Dasta JF. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. et al.
- Stollings JL, Thompson JL, Ferrell BA, Scheinin M, Wilkinson GR, Hughes CG. Sedative Plasma Concentrations and Delirium Risk in Critical Illness. Ann Pharmacother. 2018;52(6):513–21. doi: 10.1177/1060028017753480. et al.
- Taskforce DAS, Baron R, Binder A, Biniek R, Braune S, Buerkle H. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision. 2015;2015;13 doi: 10.3205/000223. et al. (DAS-Guideline). Ger Med Sci. Doc19.
- Tonner P. To boldly go where no man has gone before. Intensetimes. 2016;26:2.
- Shehabi Y, Chan L, Kadiman S, Alias A, Ismail WN, Tan MA. Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive Care Med. 2013;39(5):910–8. doi: 10.1007/ s00134–013–2830–2. et al.]
- Brochard L. Less sedation in intensive care: the pendulum swings back. Lancet. 2010;375(9713):436–8. doi: 10.1016/S0140–6736(10)60103–1.
- Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. New England Journal of Medicine. 2000;342:1471–7. doi: 10.1056/NEJM200005183422002.
- Strom T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet. 2010;375(9713):475– 80. doi: 10.1016/S0140–6736(09)62072–9.
- Dundee JW, Halliday NJ, Harper KW, Brogden RN. Midazolam: a review of its pharmacological properties and therapeutic use. Drugs. 1984;28(6):519–543. doi: 10.2165/00003495–198428060–00002.
- Aaron Conway, John Rolley, Joanna R Sutherland, Cochrane Emergency and Critical Care Group Midazolam for sedation before procedures Cochrane Database Syst Rev. 2016 May; 2016(5): CD009491. Published online 2016 May 20.
- Junkai Wang, Pei Sun, Peipeng LiangNeuropsychopharmacological effects of midazolam on the human brain Brain Inform. 2020 Dec; 7(1): 15. Published online 2020 Nov 10. doi: 10.1186/s40708–020–00116-y
- Qi Chen, Lufei Wang, Lina Ge, Yuan Gao, Hang Wang The Anxiolytic Effect of Midazolam in Third Molar Extraction: A Systematic Review PLoS One. 2015; 10(4): e0121410. Published online 2015 Apr 7.
- Rikuo Masuda, Mutsumi Nonaka, Akiko Nishimura, Kinuko Gotoh, Shuichirou Oka, Takehiko Iijima. Optimal and safe standard doses of midazolam and propofol to achieve patient and doctor satisfaction with dental treatment: A prospective cohort study PLoS One. 2017; 12(2): e0171627. Published online 2017 Feb 9.
- Soeun Jeon, Hyeon-Jeong Lee, Wangseok Do, HaeKyu Kim, Jae-Young Kwon, Boo Young Hwang, Jihwan YunRandomized controlled trial assessing the effectiveness of midazolam premedication as an anxiolytic, analgesic, sedative, and hemodynamic stabilizer Medicine (Baltimore) 2018 Aug; 97(35): e12187. Published online 2018 Aug 21. doi: 10.1097/ MD.0000000000012187
- Jennifer E. Ross, Emily Vertosick, Michael Long, Christian Cansino, Melissa Assel, Rebecca TwerskyMidazolam’s Effect on Post Operative Nausea and Vomiting and Discharge Times in Outpatients Undergoing Cancer Related Surgery AANA J. Author manuscript; available in PMC 2020 Jun 1. Published in final edited form as: AANA J. 2019 Jun; 87(3): 179–183.
- Michael C Grant 1, Jimin Kim, Andrew J Page, Deborah Hobson, Elizabeth Wick, Christopher L Wu The Effect of Intravenous Midazolam on Postoperative Nausea and Vomiting: A Meta-Analysis Anesth Analg. 2016 Mar;122(3):656–63. doi: 10.1213/ ANE.0000000000000941.
- Eun Jin Ahn, Hyun Kang, Geun Joo Choi, Chong Wha Baek, Yong Hun Jung, Young Choel WooThe Effectiveness of Midazolam for Preventing Postoperative Nausea and Vomiting: A Systematic Review and Meta-Analysis Anesth Analg 2016 Mar;122(3):664–76. doi: 10.1213/ANE.0000000000001062.
- Rodola F. Midazolam as an anti-emetic. Eur Rev Med Pharmacol Sci. 2016;10:121–126.
- Wilson S, Meyer H, Fecho K. Postoperative nausea and vomiting after inpatient and outpatient breast surgery: Incidence and effects of midazolam. Ambulatory Surgery. 2009;15(4):68–72.
- Qadirullah M, Iqbal Z. Postoperative nausea and vomiting in ambulatory surgery: Comparison of midazolam with normal saline. J Med Sci. 2016; 24(3):149–154.
- Bauer KP, Dom PM, Ramirez AM, O’Flaherty JE. Preoperative intravenous midazolam: Benefits beyond anxiolysis. J Clin Anesth. 2004;16(3):177–83.
- Eric Prommer Midazolam: an essential palliative care drug Palliat Care Soc Pract. 2020; 14: 2632352419895527. Published online 2020 Jan 13. doi: 10.1177/2632352419895527
- Huang Y, Deng Y, Zhang R, Meng M, Chen D. Comparing the Effect of Dexmedetomidine and Midazolam in Patients with Brain Injury. .Brain Sci. 2022 Jun 8;12(6):752. doi: 10.3390/brainsci12060752.
- Soeun Jeon, Hyeon-Jeong Lee, Wangseok Do, HaeKyu Kim, Jae-Young Kwon, Boo Young Hwang, Jihwan Yun Randomized controlled trial assessing the effectiveness of midazolam premedication as an anxiolytic, analgesic, sedative, and hemodynamic stabilizer Medicine (Baltimore). 2018 Aug;97(35):e12187. doi: 10.1097/MD.0000000000012187
- El Kenany S, Elshehawi ME, Farid AM, Eid MI. Efficacy of Adding Midazolam to Bupivacaine for Transversus Abdominis Plane Block on Postoperative Analgesia after Hysterectomy: A Randomized Controlled Study. Anesth Essays Res. 2019 JulSep;13(3):522–527. doi: 10.4103/aer.AER_95_19.
- Aaron Conway, Kristina Chang, Sebastian Mafeld, Joanna Sutherland. Midazolam for sedation before procedures in adults and children: a systematic review update Syst Rev 2021 Mar 5;10(1):69. doi: 10.1186/s13643–021–01617–5.
- K T Olkkola J Ahonen Midazolam and other benzodiazepines Handb Exp Pharmacol . 2008;(182):335– 60. doi: 10.1007/978–3-540–74806–9_16.
- Martine Ditlev, Erik Loentoft, Lisbet R Hölmich Breast augmentation under local anesthesia with intercostal blocks and light sedation J Plast Surg Hand Surg. 2022 May 5;1–8. doi: 10.1080/2000656X.2022.2069789. Online ahead of print.
- Masahiro Katsurada, Motoko Tachihara, Naoko Katsurada et al. Randomized single-blind comparative study of the midazolam/pethidine combination and midazolam alone during bronchoscopy. BMC Cancer. 2022 May 12;22(1):539. doi: 10.1186/s12885– 022–09640-y.
- ncbi.nlm.nih.gov/?term=Dossa+F&cauthor_id=31926966 Fahima Dossa, Braeden Medeiros, Christine Keng, Sergio A Acuna, Nancy N Baxter Propofol versus midazolam with or without short-acting opioids for sedation in colonoscopy: a systematic review and meta-analysis of safety, satisfaction, and efficiency outcomes Gastrointest Endosc . 2020 May;91(5):1015–1026.e7. doi: 10.1016/j. gie.2019.12.047. Epub 2020 Jan 10.
- Rongzan Zhang, Quan Lu, Younong Wu The Comparison of Midazolam and Propofol in Gastrointestinal Endoscopy: A Systematic Review and Meta-analysis Surg Laparosc Endosc Percutan Tech. 2018 Jun;28(3):153–158. doi: 10.1097/ SLE.0000000000000532.
- Hyunjee Kim, Sung-Sik Park, Jihye Shim Differences in midazolam premedication effects on recovery after short-duration ambulatory anesthesia with propofol or sevoflurane for gynecologic surgery in young patients: A randomized controlled trial Medicine (Baltimore) . 2020 Nov 20;99(47):e23194. doi: 10.1097/MD.0000000000023194.
- Jiyoung Lee, In Kyong Yi, Jung Youn Han et al. Effect of Adding Midazolam to Dual Prophylaxis for Preventing Postoperative Nausea and Vomiting J Clin Med . 2021 Oct 22;10(21):4857. doi: 10.3390/ jcm10214857.
- Orathy Patangi Sanjay. Midazolam: an effective antiemetic after cardiac surgery–a clinical trial. Anesth Analg. 2004 Aug;99(2):339–43
- Zhang Y, Li C, Shi J, Gong Y, Zeng T, Lin M, Zhang X Comparison of dexmedetomidine with midazolam for dental surgery: A systematic review and meta-analysis .Medicine (Baltimore). 2020 Oct 23;99(43):e22288. doi: 10.1097/ MD.0000000000022288.
- Taneja S, Jain A Systematic review and meta-analysis comparing the efficacy of dexmedetomidine to midazolam as premedication and a sedative agent in pediatric patients undergoing dental procedures..Oral Maxillofac Surg. 2022 Jun 27. doi: 10.1007/s10006–022–01087–6. Online ahead of print.PMID: 35759132 Review.
- Pourabbas R, Ghahramani N, Sadighi M, Pournaghi Azar F, Ghojazadeh Effect of conscious sedation use on anxiety reduction, and patient and surgeon satisfaction in dental implant surgeries: A systematic review and meta-analysis.M.Dent Med Probl. 2022 Jan-Mar;59(1):143–149. doi: 10.17219/dmp/141868.
- R Adams 1, G T Brown, M Davidson, E Fisher, J Mathisen, G Thomson, N R Webster Efficacy of dexmedetomidine compared with midazolam for sedation in adult intensive care patients: a systematic review. Br J Anaesth 2013 Nov;111(5):703–10. doi: 10.1093/bja/aet194. Epub 2013 Jun 7.
- A Bayat1, G Arscott Continuous intravenous versus bolus parenteral midazolam: a safe technique for conscious sedation in plastic surgery Br J Plast Surg. 2003 Apr;56(3):272–5. doi: 10.1016/ s0007–1226(03)00110–3. Affiliations expand PMID: 12859924 DOI: 10.1016/s0007–1226(03)00110–3
- Wang Z, Hu Z, Dai T. The comparison of propofol and midazolam for bronchoscopy: A meta-analysis of randomized controlled studies Medicine (Baltimore). 2018 Sep;97(36):e12229. doi: 10.1097/ MD.0000000000012229.
- Eugene Ng,, Anna Taddio, Arne Ohlsson Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit Cochrane Database Syst Rev. 2017 Jan 31;1(1):CD002052. doi: 10.1002/14651858.CD002052.pub3.
- Linda G. Franken, Brenda C. M. de Winter, Anniek D. Masman, Monique van Dijk, Frans P. M. Baar, Dick Tibboel, Birgit C. P. Koch, Teun van Gelder, Ron A. A. Mathot Population pharmacodynamic modelling of midazolam induced sedation in terminally ill adult patients Br J Clin Pharmacol. 2018 Feb; 84(2): 320–330. Published online 2017 Oct 26. doi: 10.1111/ bcp.13442
- Yongfang Zhou, Jie Yang, Bo Wang et al. Sequential use of midazolam and dexmedetomidine for longterm sedation may reduce weaning time in selected critically ill, mechanically ventilated patients: a randomized controlled study Crit Care. 2022; 26: 122. Published online 2022 May 3. doi: 10.1186/s13054– 022–03967–5.
- Nicola Gitti, Stefania Renzi, Mattia Marchesi, Michele Bertoni, Francisco A. Lobo, Frank A. Rasulo, Alberto Goffi, Matteo Pozzi, Simone Piva Seeking the Light in Intensive Care Unit Sedation: The Optimal Sedation Strategy for Critically Ill Patients Front Med (Lausanne) 2022; 9: 901343. Published online 2022 Jun 24. doi: 10.3389/fmed.2022.901343
- Lee SP, Sung IK, Kim JH, Lee SY, Park HS, Shim CS Efficacy and safety of flumazenil injection for the reversal of midazolam sedation after elective outpatient endoscopy. J Dig Dis. 2018 Feb;19(2):93–101. doi: 10.1111/1751–2980.12579.
- Elisabeth M H Mathus-Vliegen 1, Linda de Jong, Hedwig A Kos-Foekema Significant and safe shortening of the recovery time after flumazenil-reversed midazolam sedation Dig Dis Sci . 2014 Aug;59(8):1717–25. doi: 10.1007/s10620–014–3061– 2. Epub 2014 Feb 22.
- Nazila Sharbaf Shoar, Karlyle G. Bistas 2, Abdolreza Saadabadi 3 Flumazenil In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.2022 May 8.
- Kauppila T, Kemppainen P, Tanila H, Pertovaara A. Effect of systemic dexmedetomidine, an alpha-2 adrenoceptor agonist, on experimental pain in humans. Anesthesiology. 1991;74:3–8. doi: 10.1097/00000542–199101000–00002.
- Dollery CT, Davies DS, Draffan GH, Dargie HJ, Dean CR, Reid JL. Clinical pharmacology and pharmacokinetics of clonidine. Clin Pharmacol Ther. 1976;19(1):11–7. doi: 10.1002/cpt197619111. et al.
- Venn RM, Newman PJ, Grounds RM. A phase II study to evaluate the efficacy of dexmedetomidine for sedation in the medical intensive care unit. Intensive Care Medicine. 2003;29:201–7. doi: 10.1007/ s00134–002–1579–9.
- Strom T, Stylsvig M, Toft P. Long-term psychological effects of a no-sedation protocol in critically ill patients. Crit Care. 2011;;15(6):R293. doi: 10.1186/ cc10586.
- Olsen HT, Nedergaard HK, Strom T, Oxlund J, Wian KA, Ytrebo LM. Nonsedation or Light Sedation in Critically Ill, Mechanically Ventilated Patients. N Engl J Med. 2020;382(12):1103–11. doi: 10.1056/NEJMoa1906759. et al.
- Pichot C, Ghignone M, Quintin L. Dexmedetomidine and clonidine: from second- to first-line sedative agents in the critical care setting? J Intensive Care Med. 2012;27(4):219–37. doi: 10.1177/0885066610396815.
- Shehabi Y, Botha JA, Ernest D, Freebairn RC, Reade M, Roberts BL. Clinical application, the use of dexmedetomidine in intensive care sedation. Critical Care and Shock. 2010;13:40–50. et al.
- Pichot C, Longrois D, Ghignone M, Quintin L. Dexmédetomidine et clonidine : revue de leurs propriétés pharmacodynamiques en vue de définir la place des agonistes alpha-2 adrénergiques dans la sédation en réanimation. Annales Francaises d Anesthesie et de Reanimation. 2012;31(11):876–96. doi: 10.1016/j.annfar.2012.07.018.
- Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. Journal of the American Medical Association 2009;301:489–99.
- Akada S, Takeda S, Yoshida Y, Nakazato K, Mori M, Hongo T, et al. The efficacy of dexmedetomidine in patients with noninvasive ventilation: a preliminary study. Anesthesia and Analgesia 2008;107(1):167–70.
- Huang Z, Chen YS, Yang ZL, Liu JY. Dexmedetomidine versus midazolam for the sedation of patients with non-invasive ventilation failure. Internal Medicine 2012;51:2299–305.
- Galland C, Sergent B, Pichot C, Ghignone M, Quintin L. Acute iterative bronchospasm and ‘do not re-intubate’ orders: sedation by an alpha-2 agonist combined with noninvasive ventilation. Am J Emerg Med 2015;33(6):857 e3–5.
- Alexopoulou C, Kondili E, Diamantaki E, Psarologakis C, Kokkini S, Bolaki M, et al. Effects of dexmedetomidine on sleep quality in critically ill patients: a pilot study. Anesthesiology 2014;121(4):801–7
- Maze M. Dexmedetomidine : a view point. Drugs 2000;59:269.
- Mirski MA, Lewin JJ, 3rd, Ledroux S, Thompson C, Murakami P, Zink EK, et al. Cognitive improvement during continuous sedation in critically ill, awake and responsive patients: the Acute Neurological ICU Sedation Trial (ANIST). Intensive Care Med 2010;36(9):1505–13.
- Voituron N, Hilaire G, Quintin L. Dexmedetomidine and clonidine induce long-lasting activation of the respiratory rhythm generator of neonatal mice: possible implication for critical care. Respir Physiol Neurobiol 2012;180(1):132–40.
- Saito J, Amanai E, Hirota K. Dexmedetomidine-treated hyperventilation syndrome triggered by the distress related with a urinary catheter after general anesthesia: a case report. JA Clin Rep 2017;3(1):22
- Jakob SM, Ruokonen E, Grounds RM, Sarapohja T, Garratt C, Pocock SJ, et al. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA 2012;307(11):1151–60.
- Zhang Z, Chen K, Ni H, Zhang X, Fan H. Sedation of mechanically ventilated adults in intensive care unit: a network metaanalysis. Sci Rep 2017;7:44979.
- Belleville JP, Ward DS, Bloor BC, Maze M. Effects of intravenous dexmedetomidine in humans. I. Sedation, ventilation, and metabolic rate. Anesthesiology 1992;77(6):1125–33.
- Galland C, Ferrand FX, Cividjian A, Sergent A, Pichot C, Ghignone M, et al. Swift recovery of severe hypoxemic pneumonia upon morbid obesity. Acta Anaesthesiologica Belgica 2014;65:109–17.
- Lindgren BR, Ekstrom T, Andersson RGG. The effects of inhaled clonidine in patients with asthma. American Review of Respiratory Diseases 1986;134:266–9.
- Petitjeans F, Leroy S, Pichot C, Geloen A, Ghignone M, Quintin L. Hypothesis: Fever control, a niche for alpha-2 agonists in the setting of septic shock and severe acute respiratory distress syndrome? Temperature (Austin) 2018;5(3):224–56.
- Huang SQ, Zhang J, Zhang XX, Liu L, Yu Y, Kang XH, et al. Can Dexmedetomidine Improve Arterial Oxygenation and Intrapulmonary Shunt during One-lung Ventilation in Adults Undergoing Thoracic Surgery? A Meta-analysis of Randomized, Placebo controlled Trials. Chin Med J (Engl) 2017;130(14):1707–14.
- Nathan AT, Marino BS, Hanna B, Nicolson SC. Novel use of dexmedetomidine in a patient with pulmonary hypertension. Paediatric Anaesthesia 2008;18(8):782–4.
- Ling X, Zhou H, Ni Y, Wu C, Zhang C, Zhu Z. Does dexmedetomidine have an antiarrhythmic effect on cardiac patients? A meta-analysis of randomized controlled trials. PLoS One 2018;13(3):e0193303.
- Manolis AJ, Olympios C, Sifaki M, Handanis S, Bresnahan M, Gavras I, et al. Suppressing sympathetic activation in congestive heart failure. A new therapeutic strategy. Hypertension 1995;26(5):719–24.
- Motz W, Ippisch R, Strauer BE. The role of clonidine in hypertensive heart disease. Influence on myocardial contractility and left ventricular afterload. Chest 1983;83 (suppl):433–5.
- Quintin L, Cicala R, Kent M, Thomsen B. Effect of clonidine on myocardial ischemia : a double-blind pilot trial. Canadian Journal of Anesthesia 1993;40:85–6.
- Schraub P, Vecchi M, Matthys M, Lecomte B, Ferrara N, Ghignone M, et al. A centrally acting antihypertensive, clonidine, combined to a venous dilator, nitroglycerin, to handle severe pulmonary edema. American Journal of Emergency Medicine 2016;34(3):676.
- Geloen A, Pichot C, Leroy S, Julien C, Ghignone M, May CN, et al. Pressor Response to Noradrenaline in the Setting of Septic Shock: Anything New under the Sun-Dexmedetomidine, Clonidine? A Minireview. Biomed Res Int 2015;2015:863715.
- Singhal S, Baikati KK, Jabbour, II, Anand S. Management of refractory ascites. Am J Ther 2012;19(2):121–32
- Liepert DJ, Townsend GE. Improved hemodynamic and renal function with clonidine in coronary artery bypass grafting. Anesthesia and Analgesia 1990;70:S240.
- Chen C, Huang P, Lai L, Luo C, Ge M, Hei Z, et al. Dexmedetomidine improves gastrointestinal motility after laparoscopic resection of colorectal cancer: A randomized clinical trial. Medicine (Baltimore) 2016;95(29):e4295.
- Belhoula M, Ciebiera JP, De La Chapelle A, Boisseau N, Coeurveille D, Raucoules-Aime M. Clonidine premedication improves metabolic control in type 2 diabetic patients during ophthalmic surgery. Br J Anaesth 2003;90(4):434–9.
- Li B, Li Y, Tian S, Wang H, Wu H, Zhang A, et al. Anti-inflammatory Effects of Perioperative Dexmedetomidine Administered as an Adjunct to General Anesthesia: A Meta-analysis. Sci Rep 2015;5:12342.
- Venn RM, Newman PJ, Grounds RM. A phase II study to evaluate the efficacy of dexmedetomidine for sedation in the medical intensive care unit. Intensive Care Medicine 2003;29:201–7.
- De Backer D, Donadello K, Taccone FS, Ospina-Tascon G, Salgado D, Vincent JL. Microcirculatory alterations: potential prescription mechanisms and implications for therapy. Ann Intensive Care 2011;1(1):27
- Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care 2015;19 Suppl 3:S8.
- Morelli A, Sanfilippo F, Arnemann P, Hessler M, Kampmeier TG, D’Egidio A, et al. The Effect of Propofol and Dexmedetomidine Sedation on Norepinephrine Requirements in Septic Shock Patients: A Crossover Trial. Crit Care Med 2018.
- Ling X, Zhou H, Ni Y, Wu C, Zhang C, Zhu Z. Does dexmedetomidine have an antiarrhythmic effect on cardiac patients? A meta-analysis of randomized controlled trials. PLoS One 2018;13(3):e0193303.
- Longrois D, Petitjeans F, O Simonet, de Kock M, Belliveau M, C Pichot, Lieutaud Th, Ghignone M, Quintin L. Clinical practice: we radically alter our sedation ofcritical care patients, especially given the COVID-19 pandemics? RJAIC • 27 • 2020 • 43–76 DOI: 10.2478/rjaic-2020–0018.