The application of intravenous Parasetomol in complex therapy of pain and hypertermic syndrom in patients with polytrauma and in patients of neuroreanimation group
Donetsk National Medical University named after M.Gorkyi
Summary. In this paper the authors present the results of independent studies of the efficacy of the intravenous form of paracetamol in patients of neyroreanimatsion group with severe hyperthermic syndrome and in patients with polytrauma for correction of pain syndrome.
It was shown, that paracetomol is more effective than acelysin in complex therapy of hypertermic syndrome. Good results of application of paracetamol in a combination with narcotic analgesic are received at complex correction of a pain syndrome.
Key words: paracetomol, hyperthermic syndrome, pain syndrome.
The major objective of intensive care in neurocritical patients (severe traumatic brain injury, severe stroke, meningoencephalitis) is to maintain an optimal flow of oxygen-rich blood to the brain. Therefore, prevention and treatment of recurrent episodes of cerebral ischemia, such as secondary ischemic attacks caused by systemic and intracranial pathological processes, are of crucial significance. Systemic processes include hypotension, hypoxia, hyper- and hypocapnia, electrolyte disorders, anaemia, pyrexia, hyper- and hypoglycaemia, and the acid-base balance disturbances. Intracranial factors of secondary ischaemia include intracranial hypertension, cerebral oedema, hydrocephalus, intracranial infectious complications, seizures, etc. One of the major systemic pathological processes in this range is hyperthermia.
Hyperthermic syndrome in neurointensive patients may be caused by several factors. The development of hyperthermia due to infectious complications (aspiration syndrome, pneumonia, bedsores, phlebitis, etc.) should not be disregarded. However, the greatest risk for these patients is the so-called “central hyperthermia” as a result of hypothalamus stimulation (diencephalic syndrome). This hyperthermia requires urgent measures, because it leads to a significant increase in oxygen consumption and aggravates secondary hypoxic damage of the CNS.
An increase in the body temperature up to hyperpyretic values is characterized by changes in the functions of internal organs and their systems. Disorders of CVS function are exacerbated, and the so-called hyperthermal cardiovascular syndrome is developed, presenting with the following symptoms:
aggravated tachycardia;
decreased stroke volume;
cardiac output is provided mainly due to increased heart rate;
microcirculatory disorders;
– signs of SLUDGE syndrome, disseminated intravascular coagulation of blood proteins (DIC syndrome) and fibrinolysis; and acidosis.
The increased acidosis is accompanied by:
– elevated both ventilation and release of carbon dioxide;
– increased oxygen consumption; and decreased oxygen–haemoglobin dissociation.
The latter combined with circulatory disorders aggravates hypoxemia and hypoxia. This, in turn, causes the activation of glycolysis, and aggravations in disturbed energy supply of tissues and the degree of acidosis.
Modern trends in postoperative analgesia are characterized by the following: There has been a trend in significant limitations of the conventional use of opioid analgesics, not only because of increased requirements to strict accounting of narcotic analgesics, but also due to their low efficacy and the occurrence of adverse effects (especially in elderly and senile people), manifested in respiratory depression, hypodynamia, nausea, vomiting, urinary retention, pruritus, drug dependence and the potential for addiction;
There is a wider use of modern most effective non-opioid analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), and intravenous paracetamol. The frequency of their use varies from 45 to 99%;
A trend has been developed in the application of multimodal postoperative analgesia with the simultaneous administration of several anesthetics and adjuvant agents exerting their effects on various mechanisms of pain syndrome development and preventing adverse events caused by analgesics. There are ongoing studies on the well-balanced selection of optimal combinations of analgesics and adjuvant agents aimed at reducing the toxicity of drugs.
Paracetamol has analgesic and antipyretic effects. It inhibits cyclooxygenase I and II in the CNS, and affects pain centers and thermoregulation. It does not affect the synthesis of prostaglandin (PG) in the peripheral tissues, therefore, has no negative impact on the water-salt metabolism (sodium and water retention) and gastrointestinal mucosa. The maximum concentration (Cmax) is observed in 15 min, and amounts to 15-30 μg/mL. The volume of distribution is 1 L/kg. The drug poorly binds to plasma proteins. The drug penetrates the blood-brain barrier (BBB). The drug is metabolized in the liver, with the subsequent formation of glucuronides and sulfates. A minor portion (4%) is metabolized by cytochrome P450 to form an intermediate metabolite (N-acetyl-p-benzoquinoneimine). Under normal conditions, it is rapidly neutralized by reduced glutathione, and excreted in the urine after binding to cysteine and mercaptopurine acid.
After the intravenous dosage form became available, the drug’s value was significantly increased and indications for the use were broadened. The intravenous dosage form is far superior to tableted dosage forms in terms of safety, because of the possibility to better manage the drug plasma concentrations. This advantage is supported by practical clinical trials which have found significant variations in the plasma concentrations of paracetamol up to dangerously high levels after oral use compared to the intravenous administration.
Paracetamol depresses the “central” pathway of synthesis of prostaglandins that regulate the process of body temperature increase. The drug is prescribed in a single dose of 10-15 mg/kg.
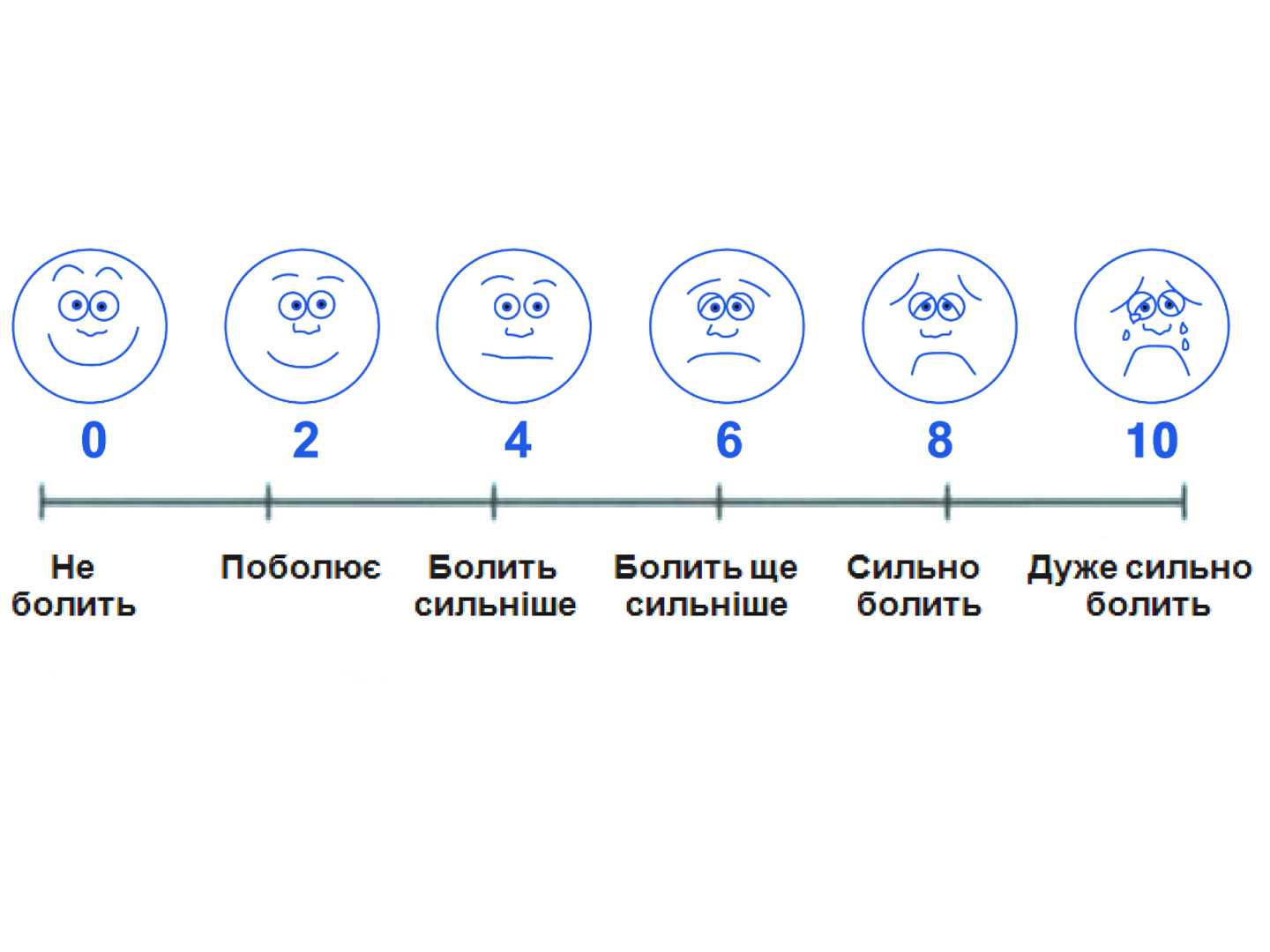
The aim of the study was to assess the efficacy of the intravenous dosage form of paracetamol in achieving an antipyretic effect in patients with central hyperthermia being treated at the anaesthesiology and intensive therapy unit (patients with traumatic brain injury, stroke), and an analgesic action in patients with multiple trauma.