The first results of the international multicenter clinical study RheoSTAT-CP0669 on the effectiveness and safety of infusion solution Rheosorbilact® in the complex treatment of patients with burns

ABSTRACT. Mechanization and urbanization are accompanied by an increase in the prevalence of burns. A burn causes both local damage and systemic inflammatory response that leads to inadequate oxygen delivery to vital organs and inadequate elimination of metabolites.
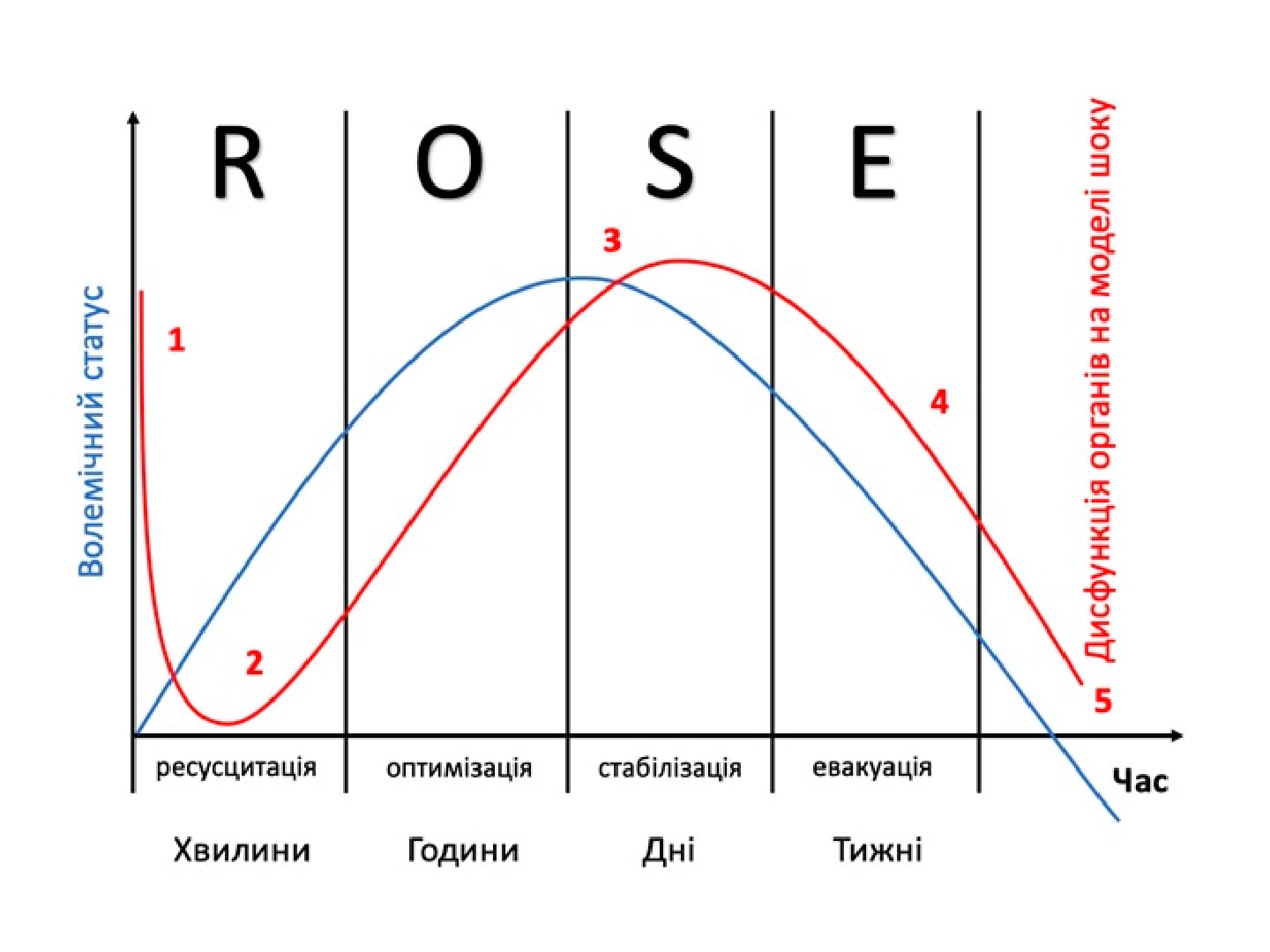
Infusion therapy for burns aims to restore perfusion and prevent ischemia. The implementation of effective dynamic schemes of infusion therapy has led to a decrease in mortality, however, an excessive amount of injected fluid does not improve the patient’s volumetric status, instead increasing tissue swelling and causing a number of complications.
Therefore, doctors are faced with the question of choosing the optimal infusion therapy, which will allow maintaining the patient’s status at the needed level called normovolemia.
According to the results of the open, blinded evaluation of the randomized controlled trial RheoSTAT-СР0669, administration of Rheosorbilact to patients with burns by intravenous infusion at a dose of 200-400 ml/day for 3 days significantly improves the clinical condition, reduces the manifestations of (poly-) organ failure and endogenous intoxication.
Small-volume infusion therapy with Rheosorbilact causes a statistically significant decrease in the breathing rate, a decrease in endogenous intoxication and the intensity of inflammation, as well as positive dynamics of the blood gas composition. Administration of the drug in this mode has a favorable safety profile: it does not lead to fluid overload, associated complications, or other serious undesirable side effects, and does not cause a clinically significant increase in blood lactate level.
The RheoSTAT-СР0669 study substantiates the feasibility of using Rheosorbilact in the complex therapy of burns.
Conflict of interest: none.
Key words: burn disease, infusion therapy, Rheosorbilact.
Authors:
- Nahaichuk Vasyl Ivanovych, Vinnytsia Regional Clinical Hospital named after M.I. Pyrogov, Vinnytsia, Ukraine
- Kozynets Heorhii Pavlovych, Kyiv City Clinical Hospital № 2, Kyiv, Ukraine
- Sharipova Visolat Khamzaevna, Republican Scientific Center of Emergency Medical Aid, Tashkent, Uzbekistan
- Chirimpey О., Republican Clinical Hospital of Traumatology and Orthopedics, Chisinau, Moldova
- Tuleubaev B., Karaganda State Medical University, Karaganda, Kazakhstan
Literature:
- World Health Organization. Burns. 2018. Available at: www.who.int/en/news-room/fact-sheets/detail/burns.
- Xiuni Z., Yuan L., Xiaohong D., Chengsong D., Yunfeng P., Ailing H. The correlation between quality of life and acceptability of disability in patients with facial burn scars. Frontiers in Bioengineering and Biotechnology. 2019; 7: 329. doi: 10.3389/fbioe.2019.00329.
- van Zuijlen P.P.M., Korkmaz H.I., Sheraton V.M., Haanstra T.M., Pijpe A., de Vries A., van der Vlies C.H., et al. The future of burn care from a complexity science perspective. Journal of Burn Care & Research. 2022; 029. doi:1093/jbcr/irac029.
- Schaefer T.J., Lopez O.N. Burn resuscitation and management. Treasure Island (FL): StatPearls Publishing, 2022.
- Guilabert P., Usúa G., Martín N., Abarca L., Barret J.P., Colomina M.J. Fluid resuscitation management in patients with burns: update. J. Anaesth. 2016; 117 (3): 284-96. doi: 10.1093/bja/aew266. PMID: 27543523.
- Jeschke M.G., van Baar M.E., Choudhry M.A., et al. Burn injury. Rev. Dis. Primers. 2020; 6: 11. doi: 10.1038/s41572-020-0145-5.
- Boehm D., Menke H. A history of fluid management – from “one size fits all” to an individualized fluid therapy in burn resuscitation. 2021; 57 (2): 187. doi: 10.3390/medicina57020187.
- Diver A.J. The evolution of burn fluid resuscitation. International Journal of Surgery. 2008; 6 (4): 345-350. doi: 10.1016/j.ijsu.2008.02.003.
- Efficacy and safety of Rheosorbilact® solution for infusion, in a complex therapy of burns. NCT04152096. Cochrane Central Register of Controlled Trials (CENTRAL). Issue 11. Available at: clinicaltrials.gov/ct2/show/NCT04152096.
- Orbegozo Cortés D., Gamarano Barros T., Njimi H., Vincent J.L. Crystalloids versus colloids: exploring differences in fluid requirements by systematic review and meta-regression. Analg. 2015; 120: 389-402. doi: 10.1213/ane.0000000000000564.
- Myburgh J.A., Mythen M.G. Resuscitation fluids. Engl. J. Med. 2013; 369: 1243-51. doi: 10.1056/NEJMra1208627.
- Gupta A.K., Asirvatham E., Reddy K., Lamba S. Fluid resuscitation in adult burns. Current Medical Issues. 2021; 19 (2): 103-109. doi: 10.4103/cmi.cmi_137_20.
- Soni N., Powell-Tuck J., Gosling P., Lobo D.N. British consensus guidelines on intravenous fluid therapy for adult surgical patients (GIFTASUP): Cassandra’s view. 2009; 64: 13-15. doi: 10.1111/j.1365-2044.2009.05886_1.x.
- Spronk P.E., Faber D.F., Rommes J.H. Effects of autotransfusion on microvascular perfusion using passive leg-raising in patients with septic shock. Chest J. 2005; 128 (4): 327S. doi: 10.1378/chest.128.4_MeetingAbstracts.376S-b.
- Epstein E.M., Waseem M. Burn resuscitation and management. Treasure Island (FL): StatPearls Publishing, 2022.
- Knaus W.A., Draper E.A., Wagner D.P., Zimmerman J.E. APACHE II: a severity of disease classification system. Care Med. 1985; 13 (10): 818-29.
- Luo Y., Wang Z., Wang C. Improvement of APACHE II score system for disease severity based on XGBoost algorithm. BMC Med. Inform. Decis. Mak. 2021; 21: 237. doi: 10.1186/s12911-021-01591-x.
- Martynoga R., Fried M. APACHE II score may predict mortality in burns patients. Care. 2009; 13: P504. doi: 10.1186/cc7668.
- Bulko I.V. Development endogenous intoxication in thermal skin burns. Natural Science Readings. 2017: 22-23.
- Wolf S.E., Rose J.K., Desai M.H., Mileski J.P., Barrow R.E., Herndon D.N. Mortality determinants in massive pediatric burns. An analysis of 103 children with > or = 80 % TBSA burns (> or = 70 % full-thickness). Surg. 1997; 225 (5): 554-65. doi: 10.1097/00000658-199705000-00012.
- Sojka J., Krakowski A.C., Stawicki S.P. Burn shock and resuscitation: many priorities, one goal. In: Stawicki S.P., Swaroop M., editors. Clinical management of shock – The science and art of physiological restoration. London: IntechOpen, 2019. Available at: www.intechopen.com/chapters/67415. doi: 10.5772/intechopen.85646.